Pre-operation
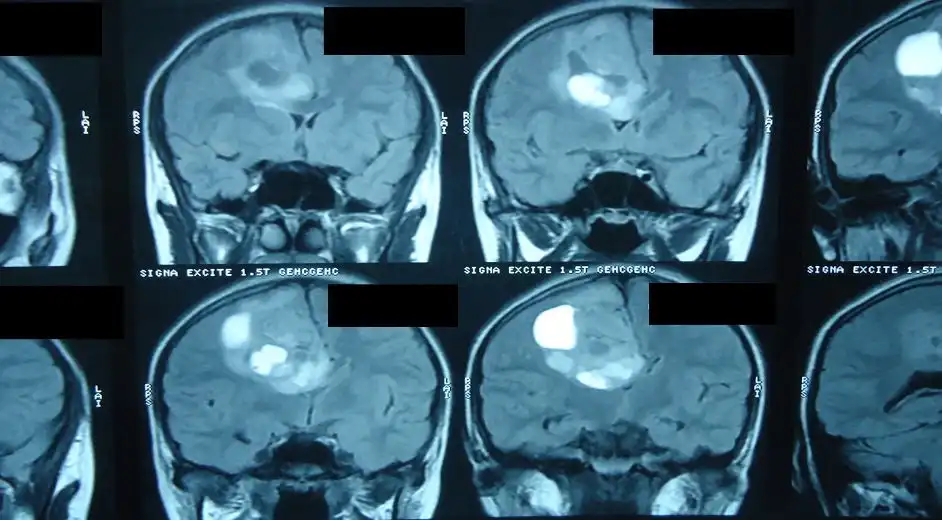
The patient is a 17-year old Kazakh girl in her last year of high school. Symptoms over the last several months included increasing weakness and difficulty coordinating her left limbs. At this point, she is still independent and able to walk. Medical investigations revealed a brain tumour more than 5 cm wide growing inside her brain, on the right parietal lobe. The brain scan above shows the position of the tumour.1. Positioning the head
The patient‘s head is placed in a special clamp in order to ensure it can‘t move.Cesnulis tells us, "Microsurgery is theoretically simple if you have the correct tools but you need to pay attention to the smallest details throughout to make sure it‘s successful. Clamping the head, for example, needs to be exceptionally precise so that it is correctly anchored in a stable position throughout the operation."
2. Positioning the neuronavigation system
The surgeon ensures the clamp is correctly positioned. Now that the head is in a stable position, the reference point for the surgical neuronavigation system is being fixed.From this reference point, a GPS pointer tracks the surface of the skin so that the surgeon knows very precisely where to go. This surgical neuronavigation system is like a very precise GPS.
The main benefits of this sophisticated mapping software are that it allows the surgeon to make the skin incision as small as possible.
Reducing the size of the craniotomy to the minimum possible significantly reduces the chance of post operative infection. It therefore helps with pain management, and is also aesthetically advantageous for the patient.
3. Mapping the tumour
In the pictures above, the surgeon adjusts the infrared camera of the neuronavigation system and registers the MRI neuronavigation system to a fixed reference point.The tumour‘s position is then projected onto the skin surface using special mapping software that allows the surgeon to see where it exactly lies under the surface, and where the eloquent areas of the brain are.
With these tools, the surgeon can plan the angle of approach in a way that avoids damaging the crucial motor areas of the brain.
In this case, there was the added challenge of working out how to avoid the tumour remnant that was located in the surgeon‘s blind spot due to the complicated access route to the tumour.
4. Preparing the area
A minimal area of the hair is shaved: this is for surgical hygiene, since there are a lot of microorganisms on the hairs that could infect the wound. The surgical area is then disinfected.Cesnulis comments that "it might seem as if the patient should have their whole head shaved in order to avoid infection, the surgeon normally only shaves as much as necessary and as little as possible, in this case, a strip along the skin incision. This approach is taken since many patients feel their hair is part of their personality - for this 17 year old girl, it might be traumatic to wake up after the operation to find her head completely shaved."














